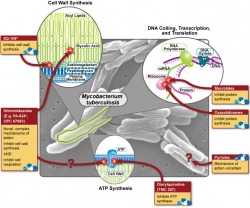
The Office of Public Health Practice hosted their annual symposium on Wednesday, and the theme was "Can the World be TB Free"? I only had a chance to attend one of the talks (by Dr. Joseph McCormick), which dealt with the rising problem of multi-drug resistant tuberculosis ( MDR-TB) and how our treatment strategies of TB may have helped this new disease to emerge. In what is sadly a familiar story for many bacterial diseases, the discovery of streptomycin (the first antibiotic that was effective against TB) was hailed as the first step in the elimination of the disease, but as time as passed the drug has become less and less effective, forcing us to search for new treatments. In the wake of the HIV/AIDS epidemic, TB has exploded and the growing problem of antibiotic resistance makes treating these people very difficult. So why does drug resistance happen, and how is it our fault? There are about 10 million (or 10^7 if you're feeling scientific) individual tuberculosis bacteria living in each cavity. About one bacteria out of every 10-100 million will randomly develop a mutation that confers resistance to any one of the two major first line drugs, rifampin and isonazid. These mutations are quite rare, but given that bacteria are nothing if not effective reproducers, it is safe to assume that approximately one bacterium per cavity is resistant to rifampin, and that another is resistant to isonazid. This situation may not sound all that bad, but consider what would happen if the patient were to be treated with rifampin alone - every single bacterium would die except for the one that had developed resistance. This bacterium is now presented with perfect growth conditions - no competition and lots of food - so it begins to multiply, and after a few days have passed, 10 million bacteria live in the cavity again - but this time all of them are resistant to rifampin. Given the large number of bacteria involved, it's now reasonable to expect that one of these resistant bacteria will then develop a resistance to isonazid, and following another single-drug treatment cycle, MDR-TB is born.
Our bodies are not our own - our intestinal tracts are colonized by an amazing variety of bacterial species - and we're just now realizing how dramatic their effect on our life truly is. A quick search shows that researchers are investigating the role of bacteria in processes as diverse as obesity, Crohn's Disease, immune suppression, blood clotting, and nutritional disorders. However, a recent talk by Dr. Vincent Denef of the University of California, Berkeley, suggests that we may be going about these investigations in the wrong way.His argument centers on the fact that two things that look alike may not act alike - and that these small differences can drastically change the ecology of entire systems. Until the advent of genomic sequencing and PCR, the only way to discover if a bacteria lived somewhere was to try to isolate it and regrow it in your lab. Unfortunately, only about 0.01% of bacteria can grow under laboratory conditions, so researchers switched to using DNA bar codes - they found a certain DNA sequence served that as a unique "fingerprint" for different species. Or so they thought. Dr. Denef has shown that even bacteria with the same fingerprint can have slightly different genomic profiles, and that these different profiles can change the bacterial composition. To put the idea of small genetic differences leading to large changes in phenotype and ecology, consider that the genomes of humans and chimpanzees are 99.9% similar - but that differing 0.01% makes a world of difference. Do these types of difference matter in bacteria? The answer is a resounding yes. One all-too-common example of small differences within the same species is antibiotic resistance. Not all strains of Staphylococcus aureus (the bug that causes staph infections) are harmful, and most people's skin is permanently colonized with these bacteria to no ill effect. But if you get infected with MRSA - the drug resistant strain - it will lead to a medical emergency. However, if you compared the normal strain to the resistant stain using the same techniques we use to fingerprint bacteria, they'd come up as the same species. Antibiotic resistance is the best example in bacteria that affect humans, and right now we just don't know how common these differences are in the bacteria living in our gut. They could be common, and they could have drastic effects (imagine if these kinds of differences caused irritable bowel syndrome!) or they could just end up being a scientific curiosity. But we won't know until we look.
Sixty days ago, a novel flu strain from Mexican pigs brought the world to a minor panic. As the data started to come in, it looked as if the strain was a serious illness in young, healthy victims - the same pattern seen with the 1918 outbreak. The initial mortality rate was just under 10%, a shockingly high figure, but after the first two weeks the rate had dropped down to 1%, mostly a result of more thorough testing of those with flu-like symptoms. In that same time frame, pig farmers and the pork lobby fought to change the name from "swine flu" to "Influenza A (H1N1)", a change which the WHO adopted. While it may seem a bit silly, the name change helped to reduce panic - think about how many warnings you got to avoid eating pork (which is just silly - cooking the pork would kill the virus, and even if you ate truckloads of infected raw pork, which I don't recommend, the viral particles are not going to survive the passage through the intestinal track. Within three weeks, global coverage of H1N1 dropped to a trickle. If the virus is mentioned today, it is usually in connection with the first death in a new country.
Ironically, the situation has worsened since the 24-hour coverage stopped. On June 11, 2009, the WHO declared a pandemic (a global epidemic). While this sounds scary, it just means that spreading in more than one global region (and the way that they define global regions is quite screwy) which cannot be traced back to a direct chain of person-to-person transmission. This criterion is easy to meet, and if you go back and look through the data (which the WHO has here), you can see that the conditions for a Level 6 pandemic were met at least one week before the declaration, and the WHO has admitted to waiting to make the announcement for political reasons (i.e. until the panic died down). Indeed, speculation as to when the announcement would be made was bouncing around the media for quite some time beforehand (do a search for "swine flu level 6" and look at the dates on the articles).
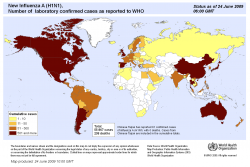
So what happens now? Is H1N1 still a threat? The answer to both questions is that we simply don't know. Flu season is over in the Northern and Southern hemispheres (where most of the developed world is located), but flu season never ends in the tropical belt - which is inhabited by a much larger percentage of the world's population. Unfortunately, this region of the world is also the one in which medical surveillance (and general medical care) is much weaker than the rest of the world - so for almost all practical purposes the virus is going to go silent for a few months before reemerging - and it will reemerge - when flu seasons begins again. For a graphic showing how severe this surveillance problem is, check out the map below (source) - it's hard to believe that the belt stretching from Southeast Asia to South Africa has so few cases (pay special attention to the scale of the colors, they are somewhat misleading - 501 cases is the same as 5,001 cases). When the virus reemerges, it could have combined with H5N1 or other flu strains, or it could have been weakened - we simply don't know and there's no real way to predict it. I agree with the WHO's generally philosophy on the issue, which is to hope for the best but prepare for the worst.
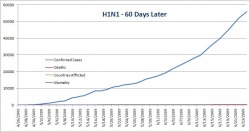
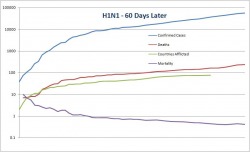
Now that we've got the background and the dangers covered, how severe has H1N1 actually been? The WHO has been kind enough to publish all of their data, including confirmed cases and mortality broken down by country ( here). I used these data to make up a graph showing confirmed cases, mortality, number of countries afflicted, and mortality rate over time. As you can see below, when you use a standard y-axis the mortality is so low that you can't even see it when compared to the overall number of cases (for the record, the mortality rate is about 0.4% - slightly higher than, but on the same order of magnitude as seasonal flu) Since using a normal axis wasn't very helpful (it's hard to extract data from a graph that you can't read) I also made a log scale graph. It looks slightly scary, but please, pay attention to the numbers on the y-axis and note that the values increase logarithmically. On this graph it's fairly easy to see that while both the confirmed cases and mortality are still climbing, the overall mortality rate is fairly constant. I attempted some curve-fitting to these lines (power regressions) but the r-value was too low for the trendlines to mean anything - so we need to wait on more data before we can make any real predictions. In this case the x-axis has the same scale as the above graph. If anyone wants the original Excel file, let me know and I'll send it to you. To conclude, I'd like to give a short caveat about this data set. It's likely that it underestimates the total number of confirmed cases (how many people with flu-like symptoms have not been tested for H1N1 around the world?), while the total number of deaths is likely to be fairly accurate - if someone dies from flu-like respiratory symptoms their blood will probably be tested. Given these two assumptions (and I stress that they are assumptions), the mortality rate may be slightly lower than the data suggest, which is certainly a Good Thing. Although we now have much more data about this pandemic virus, which appears to be much less deadly than originally feared, there's still a lot of factors that are outside of our control. What happens if the virus mutates or recombines? What effect will it have on the immuno-suppressed (AIDS victims and people with chronic parasite infections, both of which are most common in the developing world)? These are all good questions, and although we can use the data (yay epidemiology!) to help make predictions, until flu season starts again we can't say anything for certain.
With the ever-increasing use of medial imaging technology, such as CT scanning and MRI, it is now fairly common for tumors to be detected incidentally - that is, before they start to cause pain or produce symptoms on their own. While this incidental detection is a Good Thing (certainly better then only discovering a tumor after it has metastasized), in the case of small renal masses (tumors <4cm) - which can be either renal cell carcinomas (kidney cancer) or benign - the best way to treat these tumors is still a matter of (very) heated discussion. Standard procedure used to be a complete removal of the kidney - after all, we each have two, and if you remove the kidney you're guaranteed not to leave any positive margins. However, some recent studies have shown that mortality increases after a kidney is removed - even from factors not related to normal renal function. Consequently, there has been a trend towards removing part of the kidney in order to preserve renal function. Surgical intervention is an inherently risky undertaking, and despite what medical TV shows would have you believe, the average patient is not a young, attractive, generally healthy person - they are often elderly with many other comorbidities, such as heart disease. In these patients, the surgery can often be more traumatic than the disease itself.
The ideal treatment in these cases would be minimally invasive and tailored to the type, location, and size of tumor. In other words, if the tumor is benign, it doesn't make too much sense to remove it - but you often can't tell if a tumor is malignant or benign from a CT image, so you have to remove it or take a biopsy. If the tumor is malignant or high-grade (or even has the potential to become a nasty one) then it would be good to destroy it as effectively and as minimally invasively as possible.
Focal therapy attempts to answer some of these questions and it approaches the problem from two angles: the first is imaging (it's very hard to treat small tumors if you can't see them), and the second is therapeutic. The field is still controversial (most of the work I will talk about here is pretty far outside the current mainstream - if you don't believe me look at what the AUA has to say about ablative therapy) and it's still very much in its infancy. There are simply not enough data, but the research is quite exciting and the field holds huge promise. Ideally, we would like to be able to image a tumor, determine how serious (i.e. what grade) the tumor is, and preserve as much renal function as possible while sparing the patient from unnecessary stress (i.e. invasive procedures).
The ultimate in minimally invasive therapy is doing nothing - watching and waiting to see how the tumor progresses. However, growth rates don't correlate with tumor grade, so you can't distinguish a fast-growing benign lesion from a slow-growing malignant one. Next on the list are specifically targeted drugs - there is no surgery and they (in theory) only target the tumorous cells. However, there are not any approved drugs (but there are many in development) which accomplish this goal. After drugs, we move into surgical techniques - and the most accepted of these is a laparoscopic partial nephrectomy (removing part of the kidney). However, since this procedure is invasive, if a patient has multiple comorbidities it can cause severe complications. What's really needed is a step in between drugs and surgery - ablative therapy. Ablative therapy uses extreme cold (cryoablation) or extreme heat generated by radio waves (radiofrequency ablation, or RFA) to kill tumor cells. The effectiveness of these treatments remain unclear, but the idea is great - you can stick a needle through the skin into the kidney, check the placement of the needle with CT, and kill the tumor without ever cutting into the patient - and they can usually go home the next day!
My research over the summer (and what I presented on) focused solely on cryoablation - and the more we discover, the more questions we have to answer. The optimal parameters for cryoablation are still unclear (How long do we have to freeze the tumor for? How cold does it have to get? How can we find out if the cells are actually dead? Is using one needle or three needles a better treatment? What does the 5-year survival look like compared to other therapies?), but it was great to see the massive research effort that is going towards answering these basic questions. At the conference, I was constantly amazed by the caution, deliberation, and attention to detail surrounding every seemingly minor point - all to ensure that patients are treated in the best way possible. I learned a lot from the conference, and am shocked by both how much we know and how much we still have to discover in this field.
Yesterday was a fairly big day for me (but also a disappointment) - I gave my first poster presentation at an international conference (fancy, I know), and while there were only six other people (that's what I get for presenting basic research at a medical conference, the other rooms had 30-50 people in them), the presentation went well. Given that there were so few people, I felt kind of let down that I had practiced the talk so much, but all things considered, it's good that my first presentation was fairly gentle (i.e., no-one tried to stick me with too many difficult/impossible questions). So what am doing at a conference? Last summer I had the privilege to work in a medical research lab at UCI, and some of the work we did there was accepted to the conference "Focal Therapy and Imaging in Prostate and Rectal Cancer." Since the conference was in Noordwijk (near Amsterdam), I asked my PI from the summer if I could attend and present one of the posters, seeing as I was already in Europe and all. Fully expecting "No," I was suprised to find that not only did he say yes, but he thought that it would be a good opportunity.
The conference itself is different than I had expected - the first thing that jumped out at me is how much advertising and corporate sponsorship there was. After speaking with others with more experience than I (not hard to find!) it seems that this situation is fairly unique to European medical conferences, as such direct sponsorship is seen as a Bad Thing in the US, for better or for worse. Most of the time, however, is spent listening to leaders in the (admittedly niche and not yet mainstream) field of focal therapy (using extreme cold, radio frequencies, and radiation therapy to kill cancerous cells in a minimally invasive manner, i.e. "focused" on only the tumor itself) talk about advances. This workshop is giving me a skewed view of what urologists actually do - the procedures that we discuss here (and the research that I did) have not yet become the standard of care and are used mainly in patients whose cases are too complicated to perform traditional surgery (i.e. that kind of stress might kill them), but the great hope is that these minimally invasive techniques will find a broader use.
Today promises some really great events - all of which focus on renal cancer (and consequently the only day I'll have a chance of understanding a good majority of) and we even have the opportunity to see some of the most recent techniques used in two live surgery demonstrations - beamed in from operating rooms of course.
The conference venue (for some reason billed as Amsterdam) is a small resort town on the North Sea (at the opening ceremony the mayor hailed it as "the most prestigious [sic] beach resort on the North Sea" and while this might be (is) going just a bit too far, the town is nice, if a little small, and my room overlooks the ocean, so it's very hard to complain. I've even gotten to use my (extremely bad) Dutch to successfully order food.
Copper is one of those elements that we don't pay much attention to, unless we're thinking about pennies. But it's required for the production of melanin (which makes us tan), hormones (which influence our behavior), connective tissue (which holds us together), and it plays a vital role in cellular respiration and iron homeostasis (which keep us alive). In addition to all of these vital functions, copper serves as the active site of over 30 other metalloenzymes (it helps catalyze chemical reactions in the body). Copper catalyzes similar reactions in other aerobic species, including bacteria. Although it's such a necessary part of our biochemistry, too much copper can be toxic, so its cellular levels need to be well-regulated - and this balance is the focus of Dr. Marc Solioz' research at the University of Bern.
Dr. Marc Solioz presented his re at one of the Monday evening seminars at the MPI Marburg, and it's a great example of how what at first appears to be basic research into an obscure area of microbiology can have far-reaching ramifications - and if he's right, possibly even the manufacture of surgical instruments. In short, his work is the shining counterexample to those (specifically Mrs. Palin) who state that funding the basic sciences provides very little payoff.
Think of copper as a Goldilocks material - too little and biochemical reactions don't function; too much and it poisons the organism. These statements hold true for all copper-dependent organisms, from bacteria to humans. Since bacteria are fairly simple (compared to us complex organisms anyway) they make great models for studying the cellular regulation of copper. What Dr. Solioz' research shows is that bacteria regulate copper is a fairly simple way. One protein, CopA (coded by gene copA) transports copper into the cell. Another protein, CopB (coded by gene copB), transports copper out of the cell. This entire process is very finely regulated by yet another protein, CopY, which is in turn regulated by CopZ. The details of this process are not important, what is important is that a very similar process involving homologous proteins also occurs in humans.
Like all other nutrients, copper is absorbed by our intestines. From there, it is exported to the liver, which acts as a sort of warehouse, keeping some in reserve and sending the rest out to the rest of the body so that our cells can use it. If one of these pathways fails, then severe health problems result. In Menkes Disease, a human protein with 90% homology at the amino acid level in the active site to the bacterial CopB (that's very high for such a distant relationship) is faulty. Those afflicted with this mutation do not transfer copper from the small intestine to the liver - so none of the wonderful things like connective tissue and hormones receive the copper they need. This condition is always fatal, and those born with it usually die before the age of three.
Wilson's disease results from a defect in a different copper transport protein. A mutation in another CopB homologue leads to a build up of copper in the liver and brain. Since copper is toxic, this buildup causes major problems, and once a certain threshold is crossed, the liver can fail very quickly. Think of it like water backing up behind a dam - the water is not a problem until it starts to crash over the top, but then it's a big problem. In contrast to Menkes Disease, too much copper is the problem here.
So if too much copper can lead to serious health problems in humans, what happens to bacteria? In short, the same thing. Copper surfaces have been shown to kill bacteria within sixty minutes on contact - CopA brings the copper in, but there's too much for CopB to be able to export it efficiently and the resulting toxicity kills the cell. Interestingly, stainless steel, which is ubiquitous in hospitals and surgical instruments, does not exhibit any bacteriacidal properties. Hospital-acquired infections are a major problem - but if we replace the current stainless steel surfaces and instruments with ones made of copper, then Dr. Solioz' research suggests that we might be able to create a more sterile hospital environment - which might then decrease the number of hospital acquired infections. All in all, not a bad result for basic science.
Influenza, commonly known as the flu, is one of the most common viral diseases on the planet. There is a flu virus for almost every mammalian and avian species on the planets, and influenza kills approximately 36,000 people each year in the United States and hundreds of thousands worldwide. In addition to the human cost, the flu is responsible for billions of dollars in economic damage due to lost time at work and health care costs. Occasionally, flu will reach pandemic levels (a pandemic is an epidemic on a global or supra-regional scale) and can result in millions of deaths, as was the case with the 1918 Spanish Influenza (50-100 million deaths worldwide) and, more recently, the 1968 Hong Kong Influenza (~700,000 deaths worldwide).
Given that the flu is such a nasty virus under "normal" conditions, i.e., without a species-jump event, (it is likely that a species jump from birds to humans caused the 1918 pandemic), when something like swine flu starts to show up, it is a cause for concern. However, it is usually best to temper this concern with facts before it turns into a needless panic (SARS, anyone?). So what then, is the flu? To answer this question we'll have to get a bit technical, but simple explanations never work for complex problems anyway, so stick with me here and we'll see what the flu is, how it works, and why you should be concerned.
Like all viruses, the flu is pretty simple. At it's simplest level, it is a vehicle for sneaking its genetic information (the flu is an RNA virus) into host cells. The flu only has 8 genes and each gene is carried on its own segment of RNA. These segments are contained within a protein capsule comprised of the proteins hemaglutinnin and neraminidase (this is why flu strains are referred to as H1N1, H5N1, H3N2, etc.), with the hemagglutinin proteins sticking out like spikes (see figure below).
Photo Courtesy of: New York State Department of Health (here)
These spikes play a key role in infection. Their main role is to bind to sialic acid sugars found on the host cell's outer membrane, which will then lead to the virus particle being taken up by the host cell. This process is very complicated, but since different species have different sialic acid sugars, and since recognition is very specific between hemagglutinin proteins and sialic acid sugars, not every type of flu virus will be able to infect every mammilian/avian species. For example, the hemagglutinin H5 (the type found in "bird flu") can currently only recognize avian sialic acid sugars, so unless it mutates and gains the ability to recognize human sialic acid sugars it will not pose a significant threat. Swine flu, on the other hand, is an H1N1 type virus - the same type that cause the Spanish Flu pandemic, and now one of the more common flu strains - which means that it is able to infect humans fairly easily. It's best to keep in mind, however, that this H1N1 type has been around for the past century, so our immune systems are fairly well adapted to it.
Once the flu gets inside your cells, it starts to replicate. To do this, it hijacks your cellular machinery, using your proteins to replicate its genome. Once enough new virus particles have been made (about 100 million per cell), the cell will burst and these new virus particles will find new cells to infect. Normally, your immune system will recognize foreign proteins fairly quickly and produce antibodies which can destroy them. Since the hemagglutinin protein is necessary for cellular uptake, this protein is often targeted by the immune system, so it would seem that stopping the infection would be fairly trivial - just send out antibodies to destroy the hemagglutinin. However, influenza has two main factors to combat this immue reponse - a high mutation rate and scale. Like all other RNA viruses (HIV is another), influenza mutates rapidly. When this mutation rate is combined with 100 million new particles per replication cycle, every possible genome is reached quickly, which leads to some virus particles having hemagglutinin proteins that are just different enough to escape antibody detection but still specific enough to invade cells.
It's precisely these two factors that make swine flu so problematic - our immune systems have never seen this specific variant before, so it will be much harder for our immune systems to mount an effective response, which could lead to a cytokine storm (discussed in much greater detail at the link). The worst possible scenario would then be a return to the death curve seen in the Spanish Flu pandemic (see figure below), where young, healthy patients are also severely affected (the "W" shape in the solid line). As the figure shows, influenza is normally (dashed line) only fatal to the very young and very old because these groups tend to have a weaker immune system and are unable to fight off the infection. An alternate explanation for the W-shaped curve is that young, healthy people have not experienced the specific virus type before, so their immune system has no memory of it - making them susceptible to infection as well.
Graph courtesy of US Government files.
Now that we've seen why the flu does what it does and why swine flu could be a very nasty bug indeed, it's time to discuss what other factors we need to know before we let the panic set in. The first and most important factor is the mortality rate. Currently, it is estimated that 149 people in Mexico have died from swine flu, but it is not known how many were infected. If 150,000 were infected, then only 0.1% of cases are fatal (not a big deal), but if 1,500 were infected, then a staggering 10% of cases are fatal (a very big deal - mortality from the Spanish Flu pandemic is estimated to be between 2.5% - 5.0%). The lower the mortality rate, the better. Just looking at the mortality is also not enough - in order to be truly dangerous, the disease must be easily transmitted by person to person contact. If people can't spread the disease amongst themselves, then only those in close contact with infected pigs are at risk, but if sneezing can spread the disease, then you can catch it from the sick person on the bus. Sadly, the WHO has recently determined that swine flu is indeed highly transmissible - so it is smart to take precautions (see below).
Transmission rates and mortality are also not enough to accurately assess the danger - the conditions surrounding fatalities must also be taken into account. Did those that succumbed have access to hospital care? Did they even go to a hospital? Where they already immunocompromised due to AIDS or other pre-existing conditions? At this juncture there is simply not enough information to make accurate statements, so caution (but not panic) should be urged. Check the updates posted by the CDC (see the swine flu tracker at the top of this sidebar too) and the WHO as more information comes in - these organizations will be your absolute best source for reliable and up-to-date information.
The final concern is distribution. If swine flu remains localized to North America (which is looking less and less likely every day, as cases have been reported in Spain and New Zealand) then a global pandemic is less likely. However, since it has already been confirmed in Europe and Oceania it is now highly possible that it will become a global pandemic. This development is obviously a Bad Thing, as swine flu would then hit various population centers, mutate, and then make another trip around the world, a pattern seen in both the 1918 and 1968 pandemics. CNN has posted a mildly alarmist article about this, so I'll summarize briefly. Worst case scenario: 18-24 month duration, 2 billion infected, up to 7 million people dead. Being a good scientist, I'm going to have to wait a bit to make any realistic predictions, but I certainly hope that we will not see the worst case scenario. This possible crisis promises to bring a few very interesting weeks, and given the possible outcomes it would be very wise indeed to keep yourself informed. See below for things you can do and links to keep updated/learn more.
If you'd like to learn more about the flu in general, and the 1918 pandemic in particular, I highly recommend going to iTunes and checking out the two featured lectures they have under the iTunesU tab - both are free, informative, and well-made.
What Can You Do?
I am not a physician, so please, remember to be smart and not let advice on the internet supersede or worse, replace, advice from a qualified medical professional.
1. Wash your hands frequently.
2. If you're sick, stay home.
3. If you are very sick and have flu-like symptoms, see your doctor. Otherwise, stay home.
4. Avoid contact with other sick people.
5. Avoid touching your mouth, nose, and eyes after being in public.
6. If you do go to the Emergency Department, please wear a mask - if you get all of the other people there sick you will spread the virus much further and possible contaminate the whole hospital! This is not a joke; hospital-acquired infections are a leading cause of death. While wearing a surgical mask won't protect you from infection, it can prevent you from spreading the disease.
7. Don't panic - this outbreak is still in the early stages and it still too early to make any accurate predictions. Panic can only make the situation worse. If there is a significant risk, governments are likely to close schools and other public places - the best measure that they can take.
Helpful Links
What to do if you're sick with the flu
Swine Flu Updates
CDC
WHO
Flu Redux
Practical Tips for Combating Swine Flu in Your Home
So I've been trying to find a place where I can volunteer here in Marburg, and after my experience at the ER near Pomona the hospital was my first choice. The hardest part turned out to be explaining what I wanted to do, the common response being, "But you want to help? For free? What do we have to give you?" After explaining that yes, this was my goal, and no, I did not want to do an internship, everyone I talked to promptly sent me to someone else. I ended up in the social worker's office, who then told me I would have to send my CV to the head of the ER department and hope that he could provide me with something - but it would take a few weeks and there would be no guarantee.
So after this run-around I decided to change my plans - I knew that there was a Red Cross station and a Safeway (help for addicts and alcoholics) in town, but by the time I made it into town they were both closed (German opening hours, especially for anything even semi-official, are apparently random, if not based on lunar cycles). Rather dissapointed, I headed home, but on my way back stumbled across the Malteser - there's no real analogue in the US but they perform ambualtory hospice care, driving patients to hospitals, food delivery, that sort of thing. They decided to take me, pending approval by the boss (which should happen tommorrow, and which they think is likely). I'm naturally excited about this opportunity, as it will give me a chance to better my German and get more involved with the community.
On a completely different note, it looks like the Germany army is heading back to France.
So far I've had an interesting week, to say the least. Lab did not go so well on the experimental side of things - my cultures didn't grow, and without bacteria, it is difficult to extract DNA. But this setback has let me help out other people and get involved in more project, so it was not a total loss. And even as the experiments went poorly, I received confirmation that I will be attending the conference "somewhere in the Netherlands" the last weekend in Jan/first weekend February! So yay, I'll get to see what the METHECO project is all about and hear some senior scientists of the project discuss goals and progress. I will of course blog from the event/post pictures, but they may get boring to those of you who do not know/care what METHECO is (so most, if not all of the readers).
The main bad news, however is medical. Erica noticed that a mole looked slightly larger, so I went to a dermatologist. He agree that it was indeed funny, and decided to excise the "dysplastic nevus" - odd mole in non-medical English. This excision was just to be on the safe side - he is of the opinion that it is NOT skin cancer, but he sent it for lab test to be sure. However, he is not concerned, so I am not too concerned. So there is some good news there. I will of course post the results here when I get them. Bad news tho is that the excision was large enough to require stitches, so I have 5 stitches in my back now, but they are healing nicely (so far, it has been about 36 hours since I saw the doctor).
One pretty sweet cultural difference: German doctors are about as efficient as you would imagine, I called and got an appointment for within 30 minutes and did not have to wait for more than 15. He saw the mole, said it needed to be excised, and 45 min later I was out of the office. I did get to have a nice chat with him - his dad was a microbiologist/epidemiologist during "the war" (very surprising that he mentioned that) and worked to help prevent the spread of tuberculosis in Prague and the spread of tetanus in France. That is of course right up my alley with the public health and all, so the visit was not a total waste.
More exciting news: tomorrow I get to hear about filoviruses from some of the people who actually work with them in a BSL4 lab! As these researchers are rare (about 8 labs in the world are equipped to do so, and one is in Marburg) I am naturally quite excited. No more pictures this week, and we got about 8 inches (no joke) of snow today, so it would seem that winter has arrived in full force. And Erica has a website too now, so if you are interested you can check that out as well. Until next time.
|


 RSS Feed
RSS Feed